New CMS Proposed Rule
Let’s have a conversation
The Centers for Medicare and Medicaid Services (CMS), the federal oversight body for all Medicare programs, released a proposed rule on December 14, 2022, addressing policy and technical changes to the Medicare Advantage programs including Medicare Stars. Proposed rules are not final law, but they do outline what changes CMS intends to make to existing laws impacting how Medicare programs operate.
Health plans and other affected groups can submit comments to CMS for consideration by February 13, 2023, as CMS develops the final rule, which becomes law at the time of release.
Here's what you need to know about the latest proposed changes from CMS relevant to Medicare Stars.
Summary of Proposed Changes | Stars Program
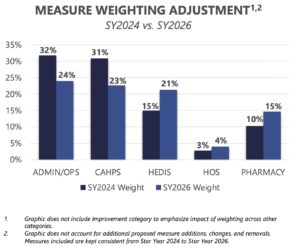
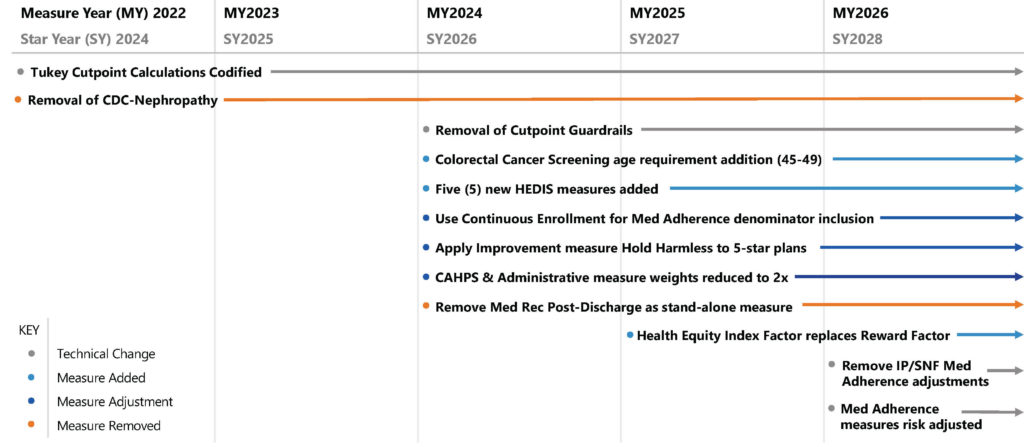
With the CY2024 Proposed Rule Changes, CMS is once again aiming to dynamically alter the Medicare Stars Quality program. The changes, only in the “proposed” stage, are subject to commentary and public review before the final rule is codified. One of the biggest changes in the proposed rules is the proposed shift of the Member Experience: Consumer Assessment of Healthcare Providers and Systems (CAHPS) and Administrative Measures from a weight of 4x back to the previous 2x weight in measurement year 2024 (Star Year 2026). This shift would have significant impacts on the relative scoring weight of the measure domains.
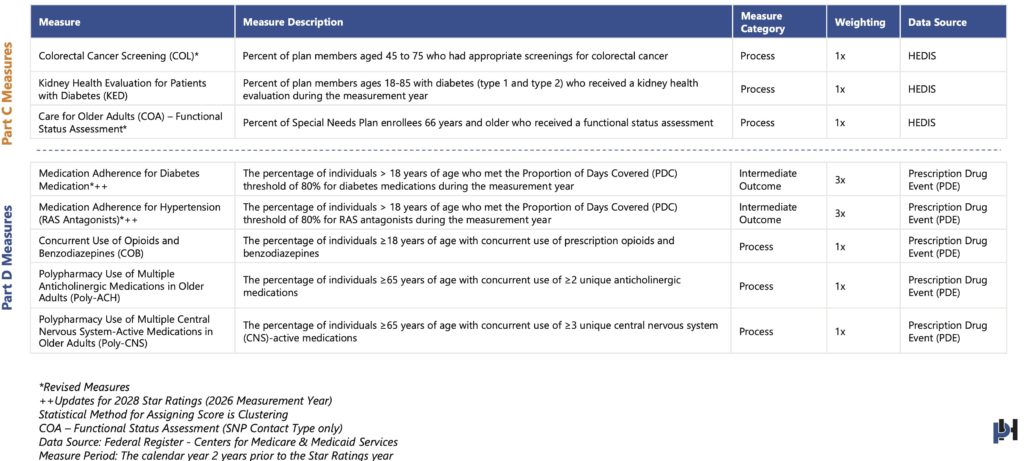
CMS is also proposing the addition of five new HEDIS and Part D measures in measurement year 2024 (Star Year 2026). These measures, listed below, will require new member-level data analysis, internal process changes, and intervention development.
- Kidney Health Evaluation for Patients with Diabetes (KED)
- Care for Older Adults (COA) Functional Status Assessment
- Concurrent use Opioids and Benzodiazepines (COB)
- Polypharmacy Use of Multiple Anticholinergic Medications in Older Adults (Poly-ACH)
- Polypharmacy Use of Multiple Central Nervous System Active Medications in Older Adults (Poly-CNS)
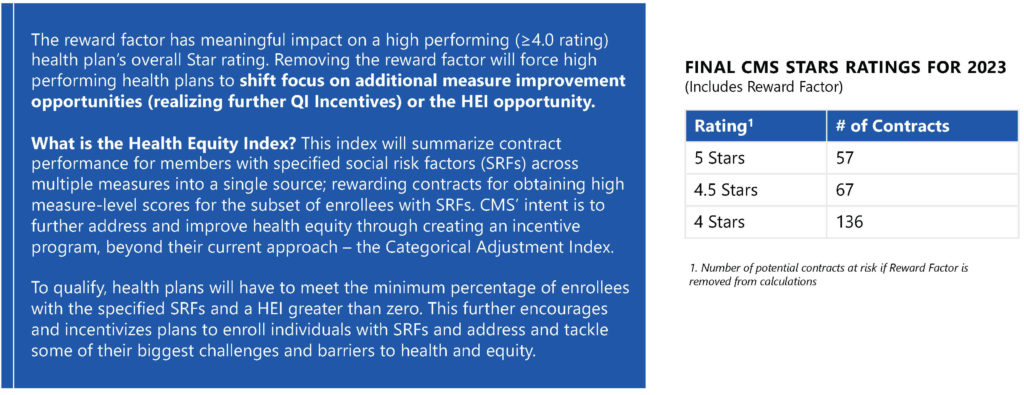
In addition to new measures and changing weight, another major proposed change from CMS is the replacement of Reward Factor with a Health Equity Index (HEI) Factor in measurement year 2025 (Star Year 2027). This change, further discussed below, will have significant impacts on the overall scoring of the Stars Program. This change will likely have disproportionate impacts on the higher scoring health plans (>4.0 Stars) given the nature of the reward factor calculation. Although much is not yet known regarding the specifics of the HEI Factor calculation, this shouldn’t come as a major shock to health plans. CMS has been signaling for some time now a commitment to health equity initiatives through quality programs, and this is very much so in line with that thinking.
Lastly, CMS is proposing the risk-adjusting at the sociodemographic level of the 3x weighted Medication Adherence measures in measurement year 2026 (Star Year 2028). These potential adjustments could have tremendous impacts to plans, especially depending on the member mix (i.e. DSNP allocation, MAPD allocation, etc.).
Weighting Shift
In Star Year(SY) 2023, CMS shifted the weight of Administrative and CAHPS measures to refocus health plan's initiatives on improving member experience. The new CMS proposed rule will reverse this change and reduce the weight of patient experience and access measures to even the weight across domains.
Weighting Shift Key Insights
Final Proposed Weighting: (MY2024/SY2026)
- Patient Experience/Complaints and Access Measures – 2x
- Process Measures – 1x
- Intermediate Outcome Measures – 3x
- Part C and D Improvement – 5x
The current 4x weighting likely caused a shift away from health-related measures and outcome driven measures given the relative weighting importance. Reducing the weighting will better align the patient experience/complaints and access measures more closely with other domains.
Plans should continue to focus interventions around listening to the voice of the member given the important link between patient experience, retention, medication adherence, and other health outcomes.
New and Revised Measures
The period of effect is beginning on or after January 1, 2024.
Replace Reward Factor with HEI
CMS is proposing to replace the reward factor with a health equity index(HEI) reward for the 2027 Star Ratings to incentivize plans to focus on improving care for enrollees with social risk factors (SRF).
Timeline Impact
Proposed Stars changes will set in starting in MY2022 (SY2024), with tiered rollout continuing through MY2026 (SY2028).
Is your health plan's Stars program ready to respond to these upcoming changes?
ProspHire’s team of Stars experts are ready to partner with your health plan to prepare and plan for these changes to the Medicare Stars program. We work shoulder to shoulder with clients to improve Star ratings and enable long-term sustainable program success.
ProspHire
216 Blvd of the Allies, Sixth Floor
Pittsburgh, PA 15222
412.391.1100
[email protected]
© 2024 ProspHire, LLC. All Rights Reserved / Terms of Use / Privacy Policy









