Understanding the 2023 Medicare Advantage Proposed Rule: Utilization Management Requirements
Let’s have a conversation
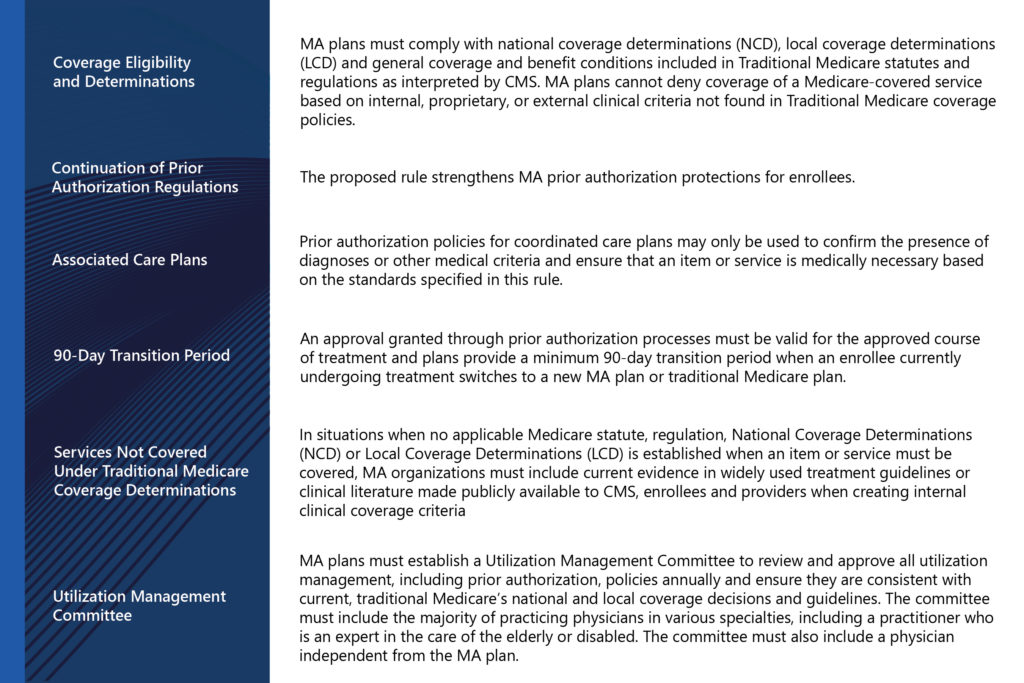
On December 14th, 2022, the Centers for Medicare & Medicaid Services (CMS) released proposed revised regulations governing Medicare Advantage (MA or Part C), the Medicare Prescription Drug Benefit (Part D), Medicare cost plans and Programs of All-Inclusive Care for the Elderly (PACE). The proposal’s focus is to increase transparency, improve health equity, reduce the cost of care and improve access to behavioral health services.
Key Medicare Advantage and Part D stakeholders will be able to provide feedback and analysis to CMS regarding the impact of these proposed changes by February 13, 2023. The proposed revisions would begin to take effect, offering guidance for the Medicare Advantage (MA) program contract year 2024.
Prior authorization can be used in a manner that results in potentially delayed patient care, burdens healthcare providers and adds unnecessary costs to the healthcare system. In summary, will focus primarily on the impact the proposed revised regulations have on utilization management and prior authorization. The effort to streamline the prior authorization process and promote healthcare is to improve the care experience across providers, patients, and caregivers.
The goal of the changes is that enrollees will receive the same access to medically necessary care they would receive in Traditional Medicare.
Key Points
What does this mean for MA plans?
For some plans, this legislative change means it is time to re-evaluate current policies and procedures in utilization management and ensure that current practices are consistent with the proposed rule. It is the time to review all existing policies and procedures related to prior authorizations, re-examine workflows and determine if staff have access and are using current traditional Medicare coverage determination materials. It is also time to establish if all coverage determination materials developed by the plan meet the requirements for development and communication. Consideration should also be given to the membership of the utilization review committee and determining if additional members are needed to cover the full scope of the specialties required to provide utilization review oversight.
How can ProspHire help
We know that a well-functioning utilization management process can improve costs, patient and provider satisfaction and compliance with regulatory requirements. With our experience in utilization review processes, policies, procedures and medical review, ProspHire can provide a baseline assessment, change management roadmap and assist with increasing efficiency, effectiveness and compliance in your utilization management functions. ProspHire focuses on best practices learned with plans across the country.
To connect with one of our experts, please fill out and submit the Contact Us Form.
ProspHire
216 Blvd of the Allies, Sixth Floor
Pittsburgh, PA 15222
412.391.1100
[email protected]
© 2024 ProspHire, LLC. All Rights Reserved / Terms of Use / Privacy Policy