Ohio Department of Medicaid calls for Exclusive Alignment through Next Generation MyCare Program
Let’s have a conversation
The Ohio Department of Medicaid (ODM) has recently initiated a significant shift in its Medicaid delivery model by inviting Managed Care Organizations (MCOs) to respond to the Next Generation MyCare Request for Applications (RFA). This new model aims to enhance care coordination and streamline health plan navigation through CMS-approved Fully Integrated Dual Eligible Special Needs Plans (FIDE SNPs). The phased implementation of the MyCare Ohio program will see the selection of no more than four MCOs to deliver these integrated services.
What is Changing?
With the introduction of the Next Generation MyCare program, ODM plans to reduce the number of participating MyCare plans from five to four, each required to provide notice to CMS of their intent to establish a FIDE SNP by Fall 2024 to align with a program start date of January 1, 2026. This change aligns with broader industry trends towards exclusive alignment and full integration of Medicare and Medicaid services.

What is the Impact?
FIDE SNPs cover Medicaid benefits (often including behavioral health), coordinate care delivery and administrative functions, cover long-term services and supports and, as of 2025, require exclusive alignment. Ohio is not the first state to adopt this model and is, in fact, following the industry trend of an increasing number of states adopting this model. The shift is expected to deliver several key benefits:
- Enhanced Care Coordination and Integration: Improved communication, data sharing and care coordination will lead to better delivery of care
- Improved Quality Measures: Metrics such as follow-up after hospitalization and medication reconciliation are anticipated to show significant improvement
- Increased Member Satisfaction: Simplified access to services and streamlined experiences will boost satisfaction
- Operational Efficiencies: Streamlined administrative processes and better resource utilization for care management and increased transparency in care coordination through data integration and sharing
Industry Trends and Legislative Support
This move mirrors nationwide trends, with an increasing number of states adopting similar models. Legislation like the DUALS Act, underscores this shift, advocating for integrated care programs that combine Medicare and Medicaid contributions, assign a single care coordinator and develop comprehensive care plans delivered by interdisciplinary care teams. Although there may be opposition from several states, this legislation indicates a significant industry shift we are seeing towards integrated care.
Regulatory Implications and Future Outlook
The Centers for Medicare & Medicaid Services (CMS) has emphasized the importance of FIDE SNP alignment in regulatory documents and are leaning on the states to help this full integration. Starting on January 1, 2030, D-SNPs will only be allowed to enroll individuals who are also enrolled in the affiliated Medicaid MCO (e.g, FIDE SNP). Additionally, SNPs must disenroll individuals not enrolled in both the D-SNP and the Medicaid MCO offered by the same parent organization. This policy will have significant impacts on organizations that provide D-SNPs but do not participate in the state's Medicaid managed care program.
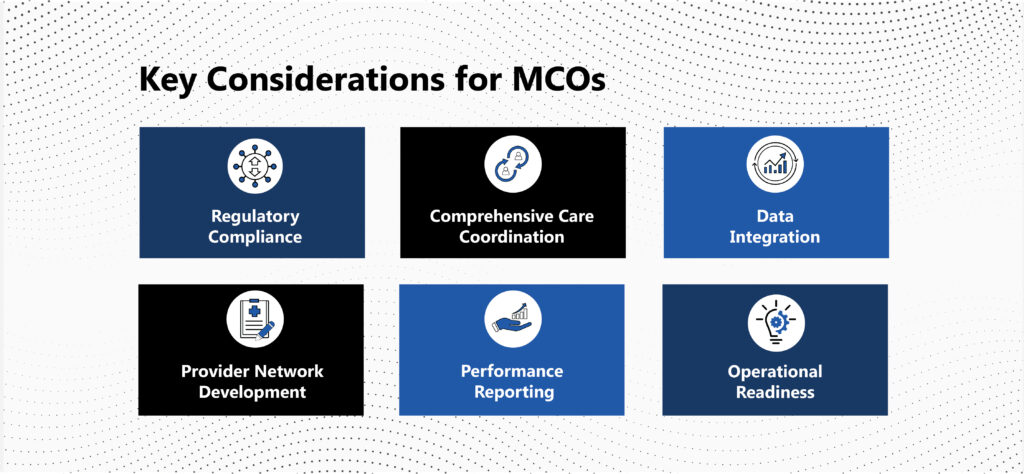
Key Considerations for MCOs
As MCO’s prepare to respond to ODM’s RFA or adopt this model, they must consider several critical factors:
- Regulatory Compliance: Adherence to across Medicare and Medicaid requirements, that vary by state, to avoid penalties and service disruptions
- Comprehensive Care Coordination: Effective care planning and risk stratification across interdisciplinary care teams
- Data Integration: Seamless data exchange process that encompasses member eligibility, claims and care management information which interfaces with state agency data for effective delivery of care and reporting
- Provider Network Development: Building an adequate network that includes Medicare and Medicaid providers, behavioral health and long-term services and supports, which often include home and community-based services
- Performance Reporting: Robust quality programs to demonstrate compliance and performance with plan requirements
- Operational Readiness: Staffing and training requirements for the unique operational requirements of a FIDE SNP combined with the complex case mix of membership lead to effective operations, implementation and continued plan performance

As a consultancy focused 100% on healthcare, ProspHire is equipped to support health plans through competitive RFAs, readiness plans and plan go-live phases. Our experienced team provides advisory services while actively executing key initiatives to deliver value. ProspHire’s expertise includes implementing state requirements for exclusive alignment, health plan growth and expansion and operational and quality performance improvements. For additional insights, connect with us today.
ProspHire
216 Blvd of the Allies, Sixth Floor
Pittsburgh, PA 15222
412.391.1100
[email protected]
© 2024 ProspHire, LLC. All Rights Reserved / Terms of Use / Privacy Policy









