Rethinking Behavioral Health and SDOH
Let’s have a conversation
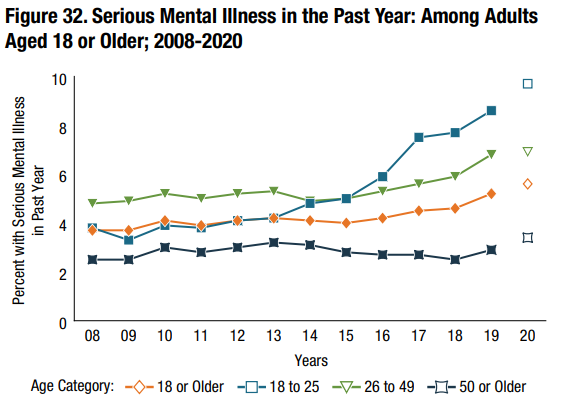
May is Mental Health Awareness Month - a reminder to all of us that checking in on your mental health is just as important as your physical health. Nationwide mental health trends reveal an increasing concern. The Substance Abuse and Mental Health Services Administration (SAMHSA) notes that one in five adults in the United States have a mental health or substance abuse disorder1. Nationwide trends in rates of mental illness reveal a rapid increase of instance over the past decade, as illustrated in Figure 1.
The American Medical Association defines behavioral health as encompassing the following conditions: mental health disorders, substance use disorders, life stressors and crises and stress-related physical symptoms2. For health plans and patients alike, often the first solution that comes to mind when addressing behavioral health issues is to focus on psychiatric interventions. Despite this assumption, mental and physical health are often intrinsically related and influenced by similar environmental factors. As a result, programs that utilize comprehensive Social Determinants of Health (SDOH) data to address behavioral health are often overlooked.
Behavioral Health and Social Determinants of Health
Social determinants, or drivers, are a useful indicator to identify factors which contribute to poor mental health in communities and individuals. Addressing health equity in all forms, including behavioral health, and SDOH factors are intrinsically related. Poor mental health can cause poor SDOH outcomes or vice versa. The National Library of Medicine3 notes that these outcomes are largely tied to food scarcity, inadequate housing, lower socioeconomic status and trauma among additional factors.
Expanding access to quality behavioral health services is a necessary component of efforts to address behavioral health and SDOH outcomes. The following indicators are associated with limited access to behavioral health services and present an opportunity for intervention:
- Health Care, including insurance coverage and provider availability
- Stable Housing - a significant contributor to mental stress
- Education, especially from an early age
- Income and Employment
- Social Support
Clinical systems are still assessing ways to measure SDOH factors to inform behavioral health policies as there are still shortfalls in assessing these metrics4. Ideally, health plans, providers and communities can partner to address these issues.
Approaches to Target Behavioral Health through SDOH
Understanding and targeting the causal factors of mental health related to SDOH is critical in enabling mental health equity. The importance of various social determinants and their continuous evidence of impact on mental health is a call to action for improved whole-person care. Housing and food access highlight the whole-person impact of SDOH on health:
Stable Housing
Inadequate and unaffordable housing can result in poor mental health5. Increased access to affordable housing and adequate living conditions present examples of interventions focused on SDOH that would directly impact mental health. Poor living conditions such as mold, lack of heating and dampness can impact both mental and physical health. Overall, a lack of affordable housing within a community causes increased rates of homelessness which can lead to even greater mental health issues and physical health risks. An intervention to offer housing programs to those with mental health illness or housing vouchers to access affordable housing are examples of efforts to drive change.
Food Security and Healthy Diet
Access to food and a healthy diet are intrinsically tied to physical health and wellness; however, evidence suggests that unhealthy eating is also a contributor to poor mental health. Having a whole-person approach to care presents a potential intervention. Individuals with illnesses such as diabetes are more likely to have depression, highlighting the correlations between mental and physical health6. Increasing food security by delivering healthy food to farmers markets, community gardens, corner stores or through home delivery offers alternative opportunities for individuals struggling with poor nutrition due to lack of access.
Evidence of successful programs continues to arise as health plans, providers and communities’ partner to address social determinants of health. Pyx Health’s Loneliness Assessment is an example of a successful intervention.
Pyx Health Loneliness Assessment
Providers can also look to interventions which work in conjunction with health plans to address behavioral health and SDOH outcomes. Pyx Health, based in Arizona, is a healthcare company which works with Medicaid and Medicare plans to support individuals experiencing loneliness. Their process involves identifying vulnerable members through SDOH screening tools and offering vulnerable members 24/7 support7. Members use the app to express their needs and are subsequently connected with resources within their health plan and community. The approach improves behavioral health outcomes and reduces stress on clinical health resources. Given the limited amount of multi-dimensional approaches which specifically address behavioral health utilizing social determinants of health, this approach serves as inspiration for similar interventions.
How ProspHire Can Help
Through ProspHire’s Addressing Health Disparities service offering, we strive to support our neighbors and clients to achieve more equitable whole-person care. Through population health assessments, targeted Social Determinant of Health interventions and innovative solutions to support behavioral health needs, we hope to enable positive change for your customers and our communities.
1 https://www.samhsa.gov/data/release/2020-national-survey-drug-use-and-health-nsduh-releases
2 https://www.ama-assn.org/delivering-care/public-health/what-behavioral-health
3 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3863696/
4 https://www.healthaffairs.org/do/10.1377/forefront.20210610.928520
ProspHire
216 Blvd of the Allies, Sixth Floor
Pittsburgh, PA 15222
412.391.1100
[email protected]
Quick Links
© 2024 ProspHire, LLC. All Rights Reserved / Terms of Use / Privacy Policy









