Community HealthChoices RFA
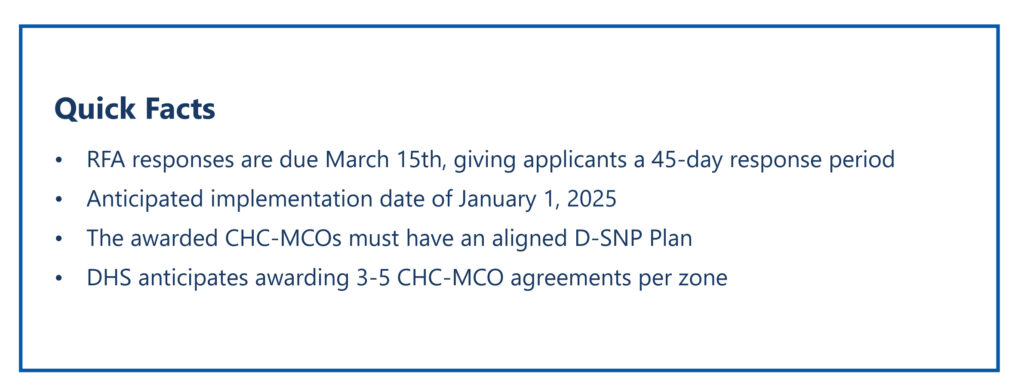
The RFA for Pennsylvania’s MLTSS services was released on January 30th, opening the door for Pennsylvania Managed Care Organizations to plans to apply to provide unique services to the 400,000+ eligible Pennsylvanians. Shifting away from statewide contracts, Community HealthChoices (CHC) awards will occur by zone, following a model similar to the physical HealthChoices program.

Since the Last RFA
Following the initial launch of the Community HealthChoices program, DHS has included notable changes to the program objectives in alignment with greater department goals going into this RFA:
- Expanding from the Triple to the Quintuple aim, reflecting improved population health and addressing health equity
- Emphasizing equity, social determinants of health and cultural competency with a “zone” approach to address the needs of Pennsylvania’s communities
- Encouragement of Participant directed model services, allowing individuals to have more control over where, when and how some of their services and supports are delivered by increasing Participant understanding of benefits
- Highlighting whole person coordinated care and community services to promote the expansion of collaborative and integrated approaches to care
- Strengthening collaboration with and coordination of behavioral health services
A Regional Approach
The governance of the CHC program is a significant change for applicants, particularly incumbents, as a criterion for this RFA is to clearly and specifically develop an approach to address the “particular and unique demographic, cultural, economic, geographic, or other relevant characteristics of the regions, counties, and municipalities comprising the zones(s)”. As a key element of the applicant’s Soundness of Approach there are several opportunities to complete an application for statewide coverage while following the technical submission opportunities to highlight the regional approach to care. This will be particularly of interest to DHS to address access to care in rural and underserved areas of the Commonwealth.

MLTSS Distinctions
While incumbents focus on program enhancements and changes, new applicants focus on adaptation of current lines of business to meet MLTSS requirements.
- Unique Provider Network: Establish or enhance provider networks by contracting with LTSS providers to meet network adequacy with cultural competency in mind, leading to new partnerships and potential value-based contracts that do not currently exist
- Person-Centered Service Plans: Develop or improve internal staffing to meet CHC requirements for care coordination, enabling tailored whole-person, or patient-centered, service plans that address participants’ needs, goals and preferences
- Rebalancing of Services: Seek to implement and enhance options for least restrictive, community-based living support for members to experience uninterrupted, patient directed, high-quality care
- Care Coordination & Integrated Services: Understand the integration of existing services (Medicare, Behavioral and MA) to enable appropriate utilization of clinical and other LTSS services, increasing member satisfaction and quality scores
Let’s have a conversation
ProspHire
216 Blvd of the Allies, Sixth Floor
Pittsburgh, PA 15222
412.391.1100
[email protected]
Quick Links
© 2024 ProspHire, LLC. All Rights Reserved / Terms of Use / Privacy Policy