Impact of NCQA Health Equity Accreditation on Medicaid Managed Care
For many years and as amplified by the impact of the COVID-19 pandemic, health plans have recognized that caring for a person’s Social Determinants of Health (SDOH) is just as important as caring for a person’s physical or behavioral health needs to result in the best outcomes for their members and improved health equity. To drive these outcomes and encourage activities focused on SDOH and health equity, state agencies are implementing regulations and contractual requirements for their Medicaid Managed Care Organizations (MCOs). In Michigan, ProspHire is seeing these regulatory requirements take hold, as the state is requiring all recently awarded Medicaid plans to obtain the National Committee for Quality Assurance’s (NCQA) Health Equity Accreditation to better care for their members. This is a trend ProspHire is seeing across multiple states, highlighting the importance of health plans awarded in a state with NCQA Health Equity requirements to remain cognizant of the amount of time and effort that goes into applying for this accreditation and act swiftly to ensure their health equity program meets the necessary criteria to avoid being penalized by the state.
What Is NCQA Health Equity Accreditation?

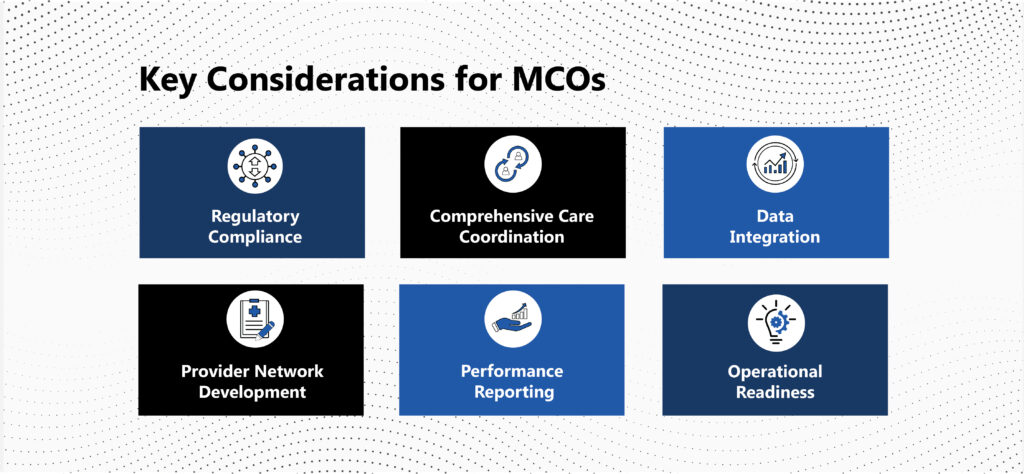
As defined by NCQA, Health Equity Accreditation focuses on the foundation of health equity work: building an internal culture that supports the organization’s external health equity work; collecting data that helps the organization create and offer language services and provider networks mindful of individuals’ cultural and linguistic needs; identifying opportunities to reduce health inequities and improve care[1]. This accreditation requires that plans submit hundreds of documents to prove to NCQA that they are compliant with the Health Equity standards and are capable of adequately caring for their members with a health equity lens. It’s also important for plans to realize that applying for Health Equity Accreditation requires immense coordination from a variety of departments such as Credentialing, Population Health and Quality.
What Are the Current Gaps Related to Health Equity and Why Are They Important for NCQA Health Equity Accreditation?

As previously noted, one state that has recently moved to require NCQA Health Equity Accreditation among their Medicaid MCOs is Michigan. In October of 2023, the Michigan Medicaid Managed Care Comprehensive Health Care Program (CHCP) RFP was released and requires that all health plans obtain NCQA Health Equity Accreditation, among other requirements[2]. For plans that don’t currently have NCQA Health Equity Accreditation, this requirement will be a major undertaking that they need to efficiently prepare for to remain compliant. As states continue to call health plans to action and seek accreditation, resources will be needed to address this significant requirement in the set timeframe.
As plans begin to work towards achieving or maintaining Health Equity Accreditation, it is important that they continue investigating the current health inequalities in their population. Continuing with Michigan as an example, one major disparity across the population is a correlation between race and the level of care received post-discharge. A 2021 study focused on 60-day outcomes for post-COVID-19 hospitalizations found that black patients had the lowest rate of follow-up post-discharge[3]. Poor follow-up post-discharge can lead to worse health outcomes and possible re-admission. Another disparity in Michigan is related to geographic location. For example, a Michigan State University study determined that there is a gap in maternity and prenatal care services in rural Michigan counties[4]. Decreased access often leads members to face a difficult decision of whether it’s worth traveling significant distances to get the care they need.
These kinds of insights can help drive health plans to create new programs to better care for their members. Using Michigan State’s findings as an example, a health plan may seek to address poor or inequitable health outcomes by offering incentives towards maternity members receiving prenatal care or credentialing additional providers in rural areas. NCQA will specifically look at how plans are tracking their member’s demographics and what programs they have created to mitigate the identified healthcare inequalities. Thus, it’s clear that continuing to collect data on the population is essential for plans to remain aware of current health inequality trends so they can adjust their programming and policies to earn or remain compliant with NCQA standards. Without proper data collection methods and adequate care programs put into place, not only will health plans not be able to receive or maintain NCQA Health Equity Accreditation, but healthcare disparities will only continue to grow.
What Is the Health Equity Accreditation Process?
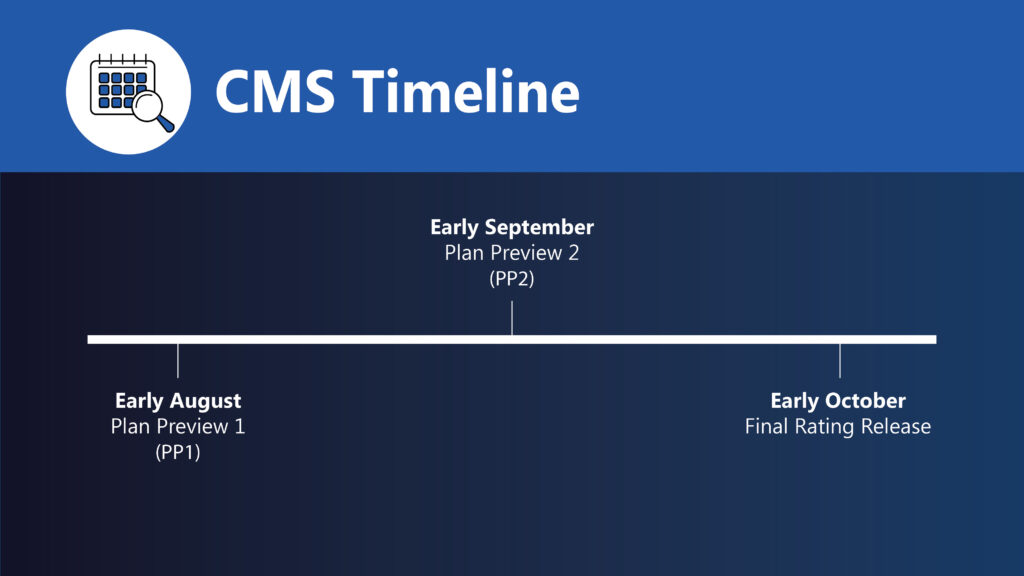
The evaluation process to receive a Health Equity Accreditation takes 9 to 12 months from when a plan submits its application to the final decision. The time frame can depend on how ready an organization is.
Here is the step-by-step application process:
- Consult with a program expert like ProspHire at least 12 months before the date you want to begin the survey.
- Buy the interactive survey tool and the standards and guidelines resource.
- Conduct a gap analysis by comparing your organization’s existing processes to the standards.
- Request a pre-application form from your program expert to start the application process.
- Submit your application.
- About 9 months before the survey date, improve your organization’s processes to match the program standards.
- Submit the survey tool about 3 months before the survey start date.
- An Accreditation Services Coordinator will review your survey submission, and the status of your accreditation will be determined within 90 days following survey submission or 30 days after the onsite file review.
Benefits of Health Equity Accreditation
Your MCO can experience several advantages from the NCQA Health Equity Accreditation, which include:
- Reduced disparities: The Health Equity Accreditation is a framework you can use to identify and address inequities among different populations, such as different races, ethnicities and gender identities. You can further analyze the data you collect and improve health outcomes for all members.
- Enhanced trust: Health Equity Accreditation signifies that you are dedicated to contributing toward health equity. This commitment can help build trust with patients, business partners, regulators and other stakeholders.
- Improved care: By addressing health disparities, you can improve the overall quality of care by identifying gaps in care and finding solutions to better meet the needs of diverse patient populations.
- Regulatory compliance: Health Equity Accreditation can help your MCO meet regulatory requirements related to health equity and cultural competency. This compliance can help reduce your risk of regulatory or state penalties.
- Operational efficiency: You can implement standardized practices to eliminate unnecessary processes and identify and establish inclusion, equity and diversity goals.
How ProspHire Can Help

Submitting for NCQA Health Equity Accreditation requires dedicated resources who are solely focused on what it takes to pass NCQA’s evaluation. Significant planning and coordination across departments is vital for the plan’s NCQA application to be successful. Plans simply can’t check a box by submitting minimal evidence to secure this accreditation. Attention to detail and going above and beyond the minimum NCQA standards is crucial to produce evidence packets that will satisfy NCQA’s criteria. Plans often do not have the time or the resources to dedicate towards NCQA accreditation, leading to costly submission delays, contract penalties and even the need to re-survey at a later date if scores aren’t high enough after the initial submission.
ProspHire is well versed in NCQA Health Equity Accreditation requirements and has been successful in achieving both the Initial and Renewal survey accreditations for their clients.
At ProspHire, we can help you understand your current state regarding health equity through data analysis and SDOH assessment. With this information, you can identify health inequities among different populations, which is crucial to understanding where to focus improvement efforts. We work with you to develop a strategic action plan that addresses disparities and aligns with Health Equity Accreditation requirements. Our dedicated partnership approach will increase your chances of successful accreditation.
Work With ProspHire to Simplify the Accreditation Process
ProspHire is committed to understanding your plan’s readiness for Health Equity Accreditation and identifying potential gaps in your survey materials. NCQA Health Equity Accreditation is a long, time-consuming process, let ProspHire help lighten the load with in-depth knowledge of the NCQA Accreditation process and extensive Health Equity experience. Contact us today for more information or to get started.
[1] NCQA | Health Equity Accreditation
[2]Health Management Associates | Michigan Medicaid RFP
[3] The Michigan Daily | Surveying Research on Racial and Ethnic Health Disparities in Michigan
[4]The Michigan Daily | Exploring Geography-Based Health Disparities in Michigan