Weathering the Storm: The Impact of Adverse Climate Events on SDOH
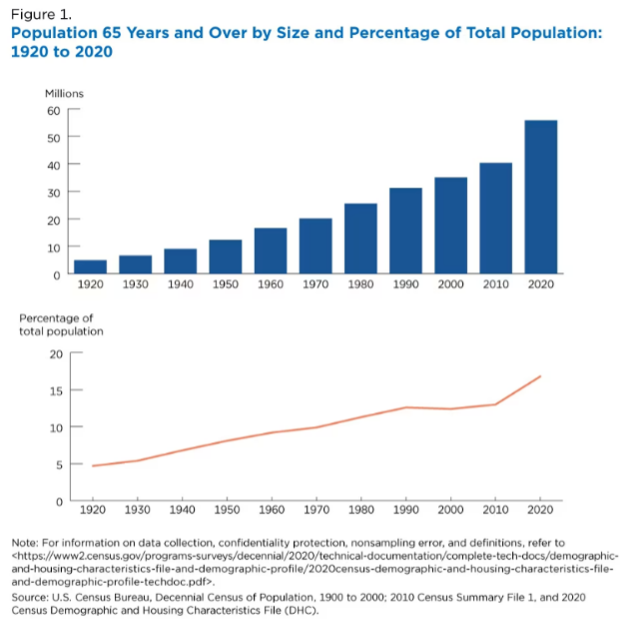
The conditions that individuals live, grow and work in can significantly impact their health outcomes and are known as the Social Determinants of Health (SDOH). SDOH factors such as economic stability, access to nutritious food and stable housing influence one’s ability to engage in healthcare and wellness and can account for up to 90% of modifiable contributors to health outcomes for a population[1].
How Do Climate Disasters Affect Your Health?
A 2021 Lancet review by editors of health journal worldwide called attention to the fact that climate change has increasingly become a significant public health threat in recent years[2]. In 2023, there have been 24 confirmed weather or climate disaster events, including wildfires, winter storms and tropical storms[3]. The National Centers for Environmental Information reported that each of these events resulted in over $1 billion in damage to public and private infrastructure including homes, schools and transportation. Individuals in these circumstances may spend months relocating or repairing their homes and may have limited access to nutritious food, clean water, education and healthcare. These disaster events affect all SDOH dimensions.
How Does Climate Change Affect Your Health?
In addition to disaster events, chronic climate change trends such as longer and hotter summers, droughts and poorer air quality are closely associated with worsening health outcomes[4]. For instance, pollen season in the U.S. increased by up to 27 days between 1995 and 2011, increasing the risk of asthma attacks in individuals with respiratory illness[5] [6]. Warmer climate conditions are also associated with increased exposure to infectious diseases. Locally transmitted cases for malaria have been identified in Florida and Texas for the first time in 20 years, leading to concerns that incidents of mosquito-borne infections can become more prevalent in the U.S. with rising temperatures[7].
A recent report estimated that the financial toll of climate change on health can add up to over $820 billion per year[8]. A large portion of this figure (~95%) is attributable to premature deaths while the rest accounts for the costs of hospitalization, treatments for mental health conditions, drugs and other healthcare services[9]. Climate change disproportionately impacts communities of lower socioeconomic status that have fewer resources available to adapt. These inequities are likely to worsen in the face of global food shortages and water scarcity, posing significant risks to population health outcomes and total cost of care.
Health strategists and organizations must start incorporating a climate change lens when planning and executing interventions to address SDOH needs. Organizations may consider including climate change preparedness into existing SDOH programs. Asthma management interventions could leverage weather forecasts and alerts to coordinate distribution of masks to at-risk pediatric members. Organizations may invest in data and analytics capabilities to predict environmental events and prioritize interventions accordingly. Health plans should build and strengthen their relationships with Community-Based Organizations that play pivotal roles during climate disasters to ensure that their members are receiving the support and care they need.

At ProspHire, we offer insights, analysis and execution strategies to address the Social Determinants of Health. Let’s have a conversation to understand the challenges your organization may face in addressing the disparate needs of underserved members across your footprint. In partnership with our clients, we develop innovative and proactive solutions to tackle the health impacts of social determinants. Connect with us today to learn more.
[1] National Academy of Medicine. (2017). Social Determinants of Health 101 for Health Care: Five Plus Five. https://nam.edu/social-determinants-of-health-101-for-health-care-five-plus-five/
[2] Call for Emergency Action to Limit Global Temperature Increases, Restore Biodiversity, and Protect Health. Lancet. (2021). https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)01915-2/fulltext#%20
[3] National Centers for Environmental Information. (2023). Billion Dollar Weather and Climate Disasters. https://www.ncei.noaa.gov/access/billions/
[4] Climate Change as a Social Determinant of Health. Pediatrics. (2020). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7193972/
[5] Asthma and Allergy Foundation of America. Climate and Health Advocacy. https://aafa.org/advocacy/key-issues/climate-and-health/
[6] Centers for Disease Control and Prevention. (2020). Allergens and Pollen. https://www.cdc.gov/climateandhealth/effects/allergen.htm
[7] The World Economic Forum. (2023). Malaria in the US – Is Climate Change Affecting Disease Spread? https://www.weforum.org/agenda/2023/07/us-malaria-climate-change-disease-transmission-dengue/
[8] National Resources Defense Council. (2021). The Costs of Inaction: The Economic Burden of Fossil Fuels and Climate Change on Health in the United States. https://www.nrdc.org/press-releases/report-health-costs-climate-change-and-fossil-fuel-pollution-tops-820-billion-year#:~:text=WASHINGTON%20%E2%80%93%20The%20staggering%2C%20often%2D,States%2C%20a%20new%20report%20shows.
[9] Six Climate Change-Related Events in The United States Accounted for About $14 Billion in Lost Lives and Health Costs. (2011). Health Affairs. https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2011.0229